How the ACIP Deviates from the USPSTF Guidelines
Preventive interventions must meet a higher safety standard than therapeutic ones—yet vaccines, though preventive, are governed by lower‑tier guidelines.
Abstract
Preventive medicine is founded on caution: interventions applied to healthy populations must exhibit near‑zero permissible risk. In therapeutic care, potential harm can sometimes be outweighed by the urgency of treating disease; in prevention, the calculus reverses—protecting the well demands tighter margins than healing the sick.
The United States Preventive Services Task Force (USPSTF) embodies this principle through an analytic framework that measures both efficacy and harm at every stage of evaluation. The Advisory Committee on Immunization Practices (ACIP), however, operates under a less rigorous paradigm. Despite vaccines being quintessential preventive agents, they are assessed using therapeutic‑tier criteria that tolerate higher risk and weaker evidentiary feedback.
This paper contrasts USPSTF’s balanced, bidirectional evidence model with ACIP’s closed‑loop structure and argues for a reformed analytic template that includes real‑world adverse outcomes, administration errors, and the documented benefits of natural infection recovery. Restoring these elements is essential if preventive medicine is to remain scientifically credible and ethically defensible.
Understanding why this inversion matters requires revisiting the moral and scientific premises that separate prevention from therapy. The two categories share clinical intent but diverge in ethical geometry: one intervenes against present harm, the other against hypothetical harm. When administrative bodies conflate them, they erase the very calculus that dictates caution in public health. USPSTF’s framework rests on respecting this boundary—quantifying benefit only after the threat of harm to healthy individuals has been stripped to its lowest real‑world level. ACIP, by contrast, appears to have collapsed that boundary entirely, adopting the tolerance of therapeutic medicine while maintaining the moral posture of prevention. To expose this shift, the first section examines the differences in risk logic that define preventive versus therapeutic interventions.
1 Introduction: Preventive vs. Therapeutic Logic
Preventive and therapeutic interventions demand fundamentally different ethical thresholds.
Preventive interventions address healthy individuals; the acceptable harm level must approach zero.
Therapeutic interventions, applied to sick patients, permit higher procedural risk because inaction itself carries danger.
Confusing these categories erodes scientific and moral integrity. When agencies extend population‑wide preventive measures without recalculating tolerable risk, prevention becomes coercive therapy in disguise.
2 USPSTF Framework: Transparent Evidence Chain
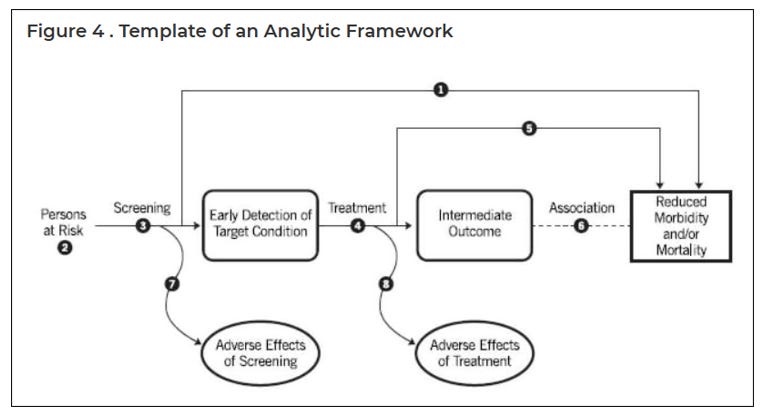
Figure 1. USPSTF Analytic Framework
The USPSTF’s analytic model tests each causal link between prevention and outcome through distinct “key questions”
Two feedback loops—Adverse Effects of Screening and Adverse Effects of Treatment—require that potential harm be measured, not theorized away.
This embedded humility defines genuine preventive science: benefit is provisional until harm data confirm safety.
3 Application Example: Breast‑Cancer Screening Conflict
USPSTF’s evidence‑bounded recommendations for biennial mammography (ages 40–74) illustrate its restraint: mortality reduction must be balanced against false positives, unnecessary biopsies, and radiation exposure.
Commercial and advocacy groups push earlier, more frequent screening, sometimes citing technological optimism. USPSTF holds its line because prevention without harm accounting is pseudoscience masquerading as care.
4 ACIP’s Functional Template: Closed‑Loop Structure
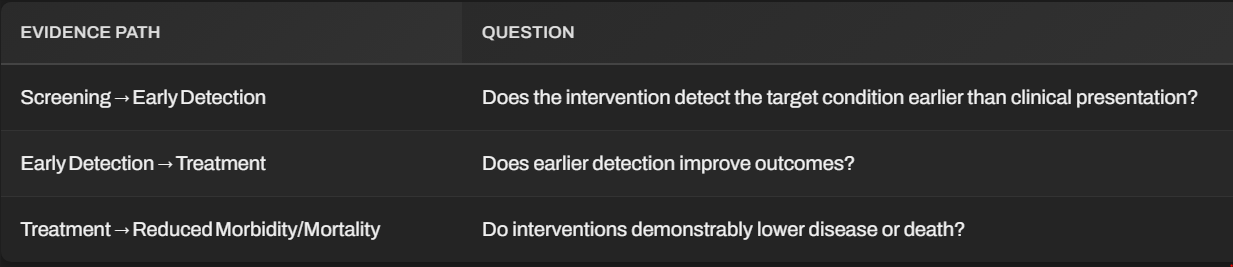
Figure 2. Current ACIP Functional Template
ACIP’s working model channels information one way:
Manufacturer‑developed studies →
FDA approval →
ACIP recommendation →
Population‑wide implementation
Post‑market surveillance (VAERS, VSD) rarely feeds back quantitatively into guideline revision.
VAERS signals are dismissed as “unverified”, VSD data locked from independent review, and known harms truncated into trivial categories (“sore arm” , “minor fever”).
This is not a learning loop—it is a confirmation loop.
5 The Missing Loops: Ignoring Predictable Error
Every mass‑injection program introduces unavoidable risk categories:
Medication substitution or contamination
Improper preparation or dosing
Expired or defective lots
Unsanitary technique
Undetected contraindications
Physiological heterogeneity (immune over‑ or under‑response)
Real‑world data confirm these occur at measurable rates even under ideal logistics.
The MMR series illustrates quantitative neglect: febrile seizure risk rises from 1 in 3,500 (MMR alone) to ≈ 1 in 1,250 (using MMRV). Fevers ≥ 102 °F occur in ≈ 20 %. Such findings would trigger USPSTF re‑evaluation; ACIP treats them as endnotes.
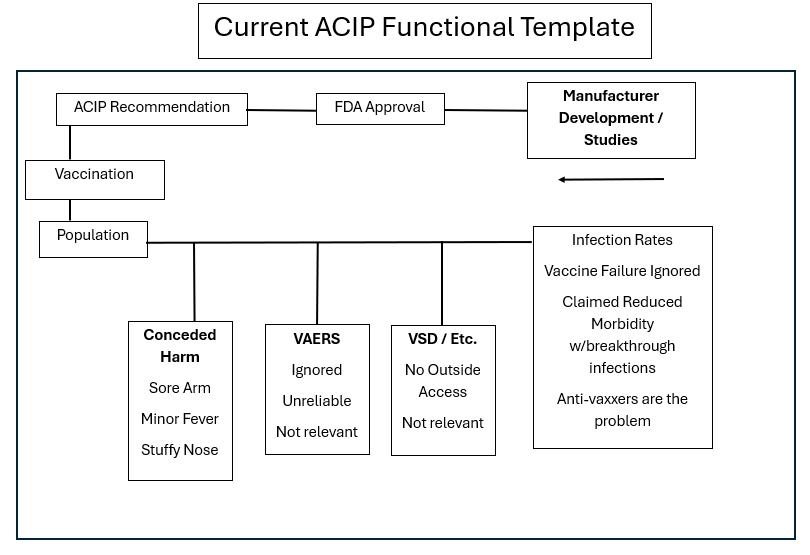
7 A Minimum Reform Template:
Restoring Symmetry
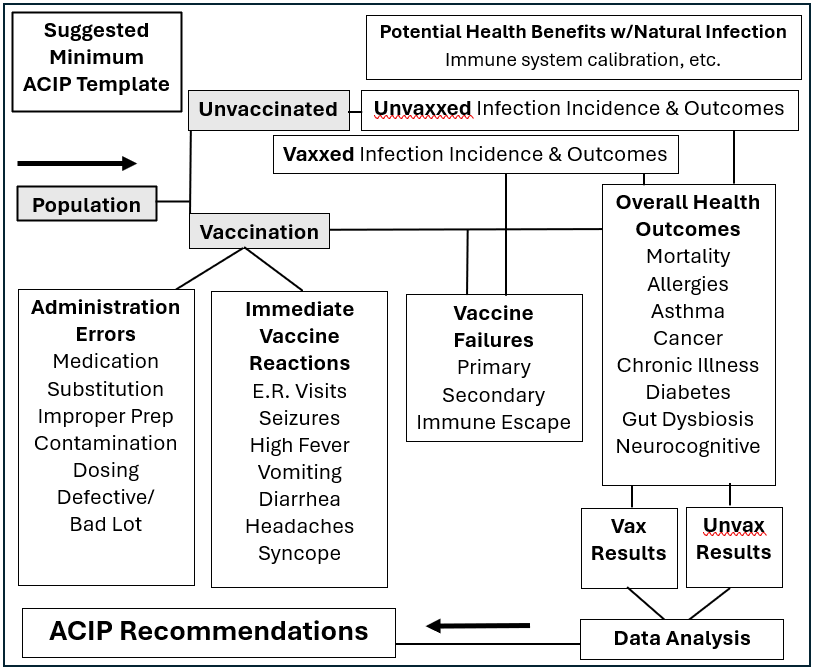
Figure 3. Suggested Minimum ACIP Template
7.1 Core Features
Dual Cohorts: Compare vaccinated and unvaccinated infection incidence and outcomes.
Explicit Error Channels: Track administration errors, immediate reactions, and vaccine failures analytic variables.
Transparent Databases: Open longitudinal datasets for independent review.
Natural Infection Recovery Node: Incorporate documented benefits—immune maturation, oncologic protection, reduced autoimmune burden—shown in Japanese and European epidemiology.
7.2 Analytic Outcome
Data flows from both cohorts into a centralized outcome box (Overall Health Outcomes”) then downward to comparative analysis and policy recommendations, (“Overall Health Outcomes”), then downward to comparative analysis and policy recommendation, mirroring USPSTF’s balanced architecture.
8 Discussion: Re‑Aligning Preventive Ethics
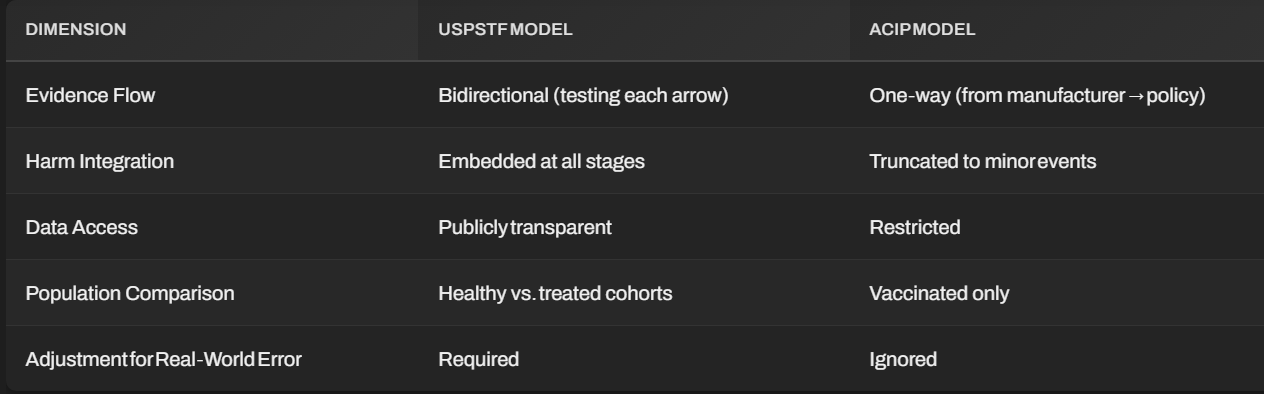
The divergence between USPSTF and ACIP marks a philosophical schism:
One treats uncertainty as a research frontier.
The other treats it as a public‑relations problem.
By internalizing adverse outcomes and alternative pathways, USPSTF practices evidence-based humility. ACIP’s model reflects bureaucratic expedience - an illusion of stability sustained by data opacity.
Reform does not undermine confidence; it earns it.
9 Conclusion
Preventive authority depends on the discipline to measure harm. USPSTF’s open‑loop analysis embodies that discipline; ACIP’s closed system does not.
Adopting a transparent, dual‑cohort architecture with mandatory harm and benefit integration would reconcile public health with scientific honesty.
When prevention ceases to test itself, it ceases to be science.

Thank you!
Cross-posted onto my 'stack. Too good a review not to share.